Clinical characteristic and pathogenesis of tumor-induced acute pancreatitis: a predictive model - BMC Gastroenterology - BMC Gastroenterology
Epidemiology
A total amount of 8970 patients were admitted for AP during the study period, and 8637 AP patients were enrolled in the study. The incidence of tumor-induced AP was 1.16% (100/8637), and the incidence was increasing year by year. Up to now, the annual incidence rates of tumor-induced AP from 2013 to 2021 were 0.29% (2/680), 0.14% (1/713), 0.25% (2/805), 0.23% (2/852), 0.46% (5/1090), 0.34% (4/1187), 0.81% (8/983), 3.82% (40/1046) and 2.81% (36/1281).
Among 3310 patients with AP from 2019 to 2021, miscellaneous causes included cholelithiasis (52.5%), hypertriglyceridemia (16.7%), idiopathic (12.7%), diet-related (9.5%), and infection (0.8%), alcohol (1.4%), autoimmune (0.4%), operation (1.5%), dialysis (0.1%), trauma (0.5%), congenital (0.1%), thrombosis (0.0%; 2 cases), pancreatolithiasis (0.5%), poisoning (0.2%), drugs (0.1%), tumor (2.4%), metastasis (0.2%), type 1 diabetes (0.0%; 2 cases), friction of drainage tube (0.0%; 2 cases), ileus (0.0%; 1 case), biliary hemorrhage after cholecystectomy (0.0%; 1 case) and familial adenomatous polyposis (0.0%; 2 cases).
Baseline clinical features
In total, 100 individuals in tumor group and 360 admissions in the non-tumor group were enrolled (mean age 56.67 ± 11.03 versus 56.36 ± 10.70 years, p = 0.000) (Table 1). Compared with the control group, the tumor group was less likely to have gallstone-related episodes as the past history. More individuals in the tumor group had multiple episodes of AP than those in the non-tumor group (59% vs 13.3%, p = 0.000). More frequent attacks of AP were in the tumor group than the control group (Z = 8.403, p = 0.000). It took 8.57 (4.29 20.36) weeks from the first episode of AP to tumor diagnosis. The diagnosis rates at 1, 2, 3 months after the first admission were 37%, 58% and 70%. When comparing to the non-tumor group, the length of stay in the tumor group was longer (Z = 5.275, p = 0.005) and the median cost during the hospitalization was more (Z = 5.474, p = 0.001), respectively.
In tumor group, progressively aggravated intense pain in the upper abdomen was special symptom of 88 patients. Of them, 23 (26.1%) patients had previous attacks of pancreatic pain before first admission. Obstructive jaundice was in 14 patients which may result from tumor itself. MAP was observed in 90 cases, MSAP in 9 cases and SAP in one case.
87 patients (87%) underwent computed tomography (CT), 69 patients (69%) underwent ultrasound (US), 47 patients (47%) underwent magnetic resonance cholangiopancreatography (MRCP), 9 patients (9%) underwent endoscopic ultrasonography (EUS) and 11 patients (11%) underwent positron emission tomography-computed tomography (PET-CT). The sensitivities of CT, US, MRCP, EUS and PET-CT were 97.7%(85/87), 84.1%(58/69), 95.7%(45/47), 100%(9/9) and 81.8%(9/11), which assessed the rate of the number of tumors detected by imaging modalities to the number of exact cases. The presentation under CT was diffuse or focal volume enlargement of the pancreas and diffuse, segmental and cystic expansion of the pancreatic ducts. US showed diffuse enlargement of pancreatic volume, reduced internal echo and unclear boundary. The sensitivity and specificity of pancreatic duct dilation were 68.0% and 91.3%. And the sensitivity and specificity of bile duct dilation were 63.3% and 92.5%. The sensitivity and specificity of double duct sign (DDS) which represented co-existence of pancreatic and bile duct dilation were 51.0% and 96.5%.
Baseline parameters of patients with different tumors
There were 73 cases located in pancreas, 13 cases in ampulla and 14 cases in extrahepatic bile duct. The clinical characteristics of patients with tumor in different sites were summarized in Table 2. Table 3 summarized the indexes with statistically significant differences by pairwise comparison. Pancreatic duct dilation was more likely to be seen in the pancreas group than the ampulla group. The sizes of the pancreas group were significantly larger than those of the biliary and ampulla group. Albumin in the pancreas group was higher than the biliary group and CEA in the pancreas group was higher than the ampulla group (all p < 0.05).
In the pancreas group, tumors mostly located in head and neck (56/73) while partly in body and tail (17/73). The comparisons of tumor characteristics in different parts of pancreas were shown in Table 4. According to pathological classification, there were 59 adenocarcinomas, 7 mucinous cystadenomas, 2 acinar cell carcinomas, 1 squamous cell carcinoma, 2 small cell carcinomas, 1 solid pseudopapilloma and 1 intraductal papilloma. Vascular invasion was observed in 14 cases. 5 cases synchronously violated portal vein and mesenteric vessels, 1 case synchronously violated liver and pancreas itself (body and tail) as well as 1 case synchronously violated psoas major and ilium. Single organ metastases included liver (17 cases), duodenum (3 cases), bone (1 case) and common bile duct (1 case). There are 27 cases (37.0%) in stage IV, 19 cases (26.0%) in stage III, 10 cases (13.7%) in stage II (3 case stage IIB and 7 case stage IIA), 17 cases (23.3%) in stage I (14 case stage IB and 3 case stage IA).
In the ampulla group, there were 6 villous tubular adenomas and 7 adenocarcinomas. Liver metastasis was observed in 1 case and biliary duct was involved in two cases. There were 3 cases (23.1%) in stage IV, 1 case (7.7%) in stage IIB and 3 cases (23.1%) in stage IB. In the biliary group, there were 12 adenocarcinomas, 1 high-grade neoplasia with canceration and 1 villous adenoma with canceration. Vascular invasion was observed in 2 cases. Single organ metastases included pancreas (1 case), duodenum (1 case) and liver (2 cases). And there were 2 cases (14.3%) in stage IV, 3 cases (21.4%) in stage III, 6 cases (42.9%) in stage II (3 case stage IIB and 3 case stage IIA) and 1 case (7.1%) in stage IB.
Totally, 32% cases were IV stage, 22% cases were III stage, 17% cases were II stage (7 case IIB and 10 case IIA) and 21% cases were I stage (18 case IB and 3 case IA). The differences among the three groups were statistically significant (p = 0.000).
Predictors for tumor-induced AP
All available features with statistical significance in Table 1 except C-reactive protein (CRP) which had many missing values, cost and time were trained by LASSO regression (Figs. 1, 2), XGB (Fig. 3) and random forest model (Fig. 4). Calibration plots and receiver operator characteristic curves were used to evaluate the model. Interestingly, all three methods revealed that age, recurrent attacks, pancreatic duct dilation, bile duct dilation, white blood cell count and percentage of neutrophils were predictors of tumor-induced AP. These variables, as age (1.05 [1.01 1.10], p = 0.013), recurrent attacks (6.19 [1.91 22.05], p = 0.003), pancreatic duct dilation (13.74 [4.04 53.29], p = 0.000), bile duct dilation (8.99 [2.42 36.57], p = 0.001), white blood cell count (0.81 [0.66 0.97], p = 0.032) and percentage of neutrophils (0.96 [0.92 1.00], p = 0.108) were calculated in logistic regression analysis and then used to develop a nomogram (Fig. 5).
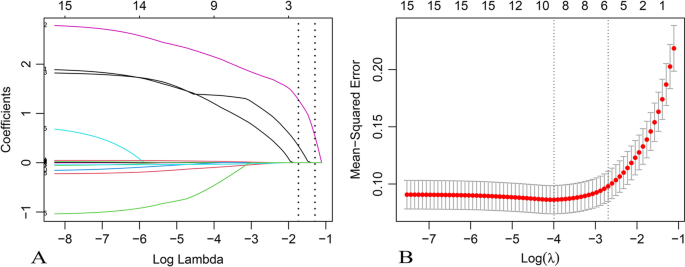
Selection of risk factors of tumor-induced AP using the LASSO logistic regression algorithm. A LASSO coefficient profiles of the 15 candidate variables. Vertical line was plotted at the given lambda, selected by tenfold cross-validation with minimum classification error and minimum classification error plus 1 standard error, respectively. For the optimal lambda that gives minimum classification error plus 1 standard error, 6 features with a non-0 coefficient were selected. B Penalization coefficient lambda in the LASSO model was tuned using tenfold cross-validation and the "lambda.1se" criterion. Area under the curve (AUC) metrics (y-axis) were plotted against log (lambda) (bottom x-axis). Top x-axis indicates the number of predictors for the given log (lambda). Red dots indicate average AUC for each model at the given lambda, and vertical bars through the red dots show the upper and lower values of the AUC according to the 10-fold cross-validation. Vertical black lines define the optimal lambda that gives the minimum classification error plus 1 standard error
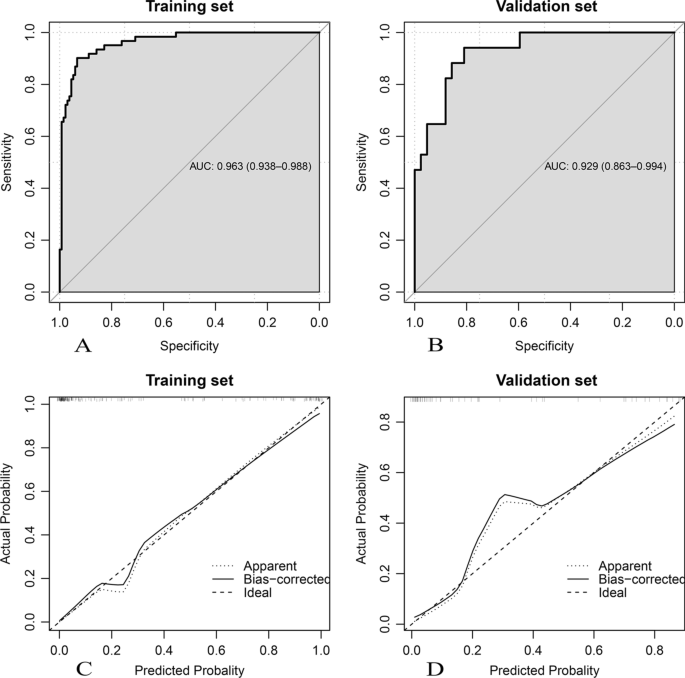
Performance of the logistic regression algorithm in tumor-induced AP prediction. (A, B) Receiver-operating characteristic curves; (C, D) calibration curves
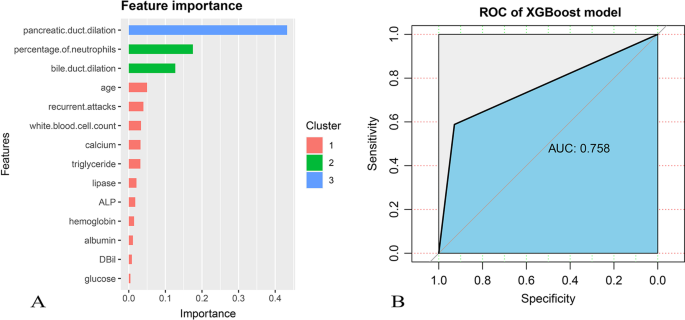
A Feature correlations and distributions of feature importance for the XGBoost model. Model input variables are ranked in descending order of feature importance. B The receiver operating characteristic curve was plotted though the test set evaluated the trained model. ALP: alkaline phosphatase; DBil: direct bilirubin
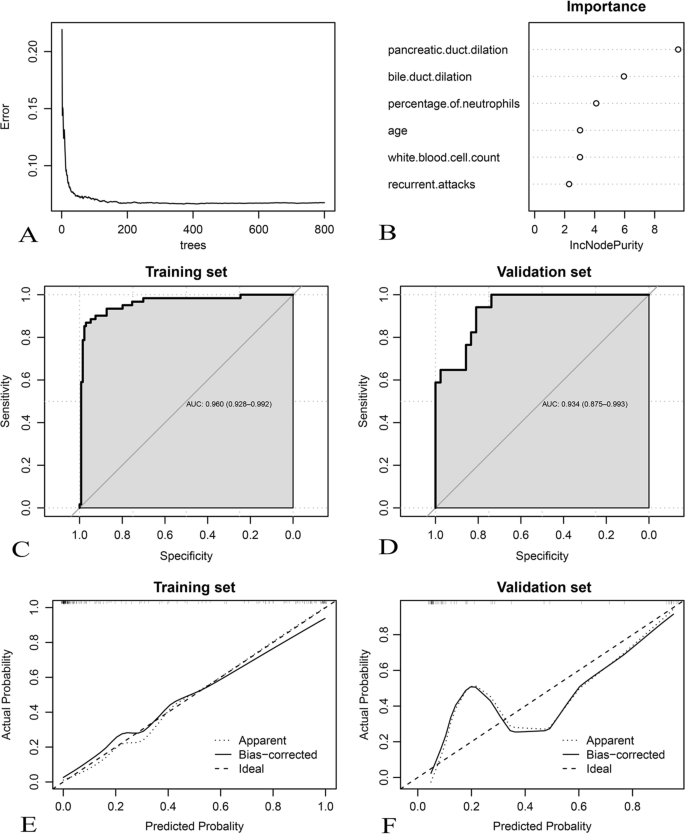
Development and assessment of the random forest algorithm in tumor-induced AP prediction. A Relationship between out-of-bag error and number of trees. In total, 139 trees are selected to establish a random forest model; B feature importance; (C, D) Receiver-operating characteristic curves; (E, F) calibration curves
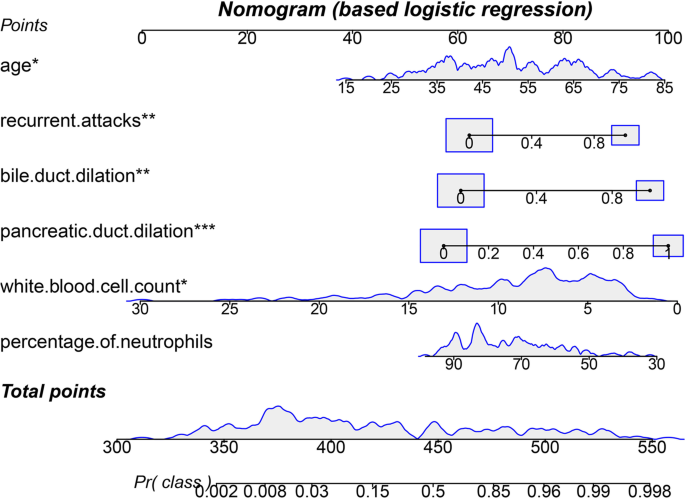
Nomogram of tumor-induced AP prediction was developed using the multivariate logistic regression model. Value assigned to each factor was scored on a scale of 0–100. By adding scores for each factor, one can obtain a total score. On the basis of the total score, the probability of tumor-induced AP is displayed by projecting the score to the bottom risk axis. *: p < 0.05; **: p < 0.01; ***: p < 0.001
Treatment and survival analysis
Endoscopic ultrasound-guided fine-needle biopsy (EUS-FNA) has performed in 7 patients. 38 patients underwent CT-guided biopsy to confirm the diagnosis. 41 patients were managed with pancreaticoduodenectomy, 13 patients underwent distal pancreatectomy, 2 underwent endoscopic ultrasound and endoscopic resection, 1 underwent endoscopic resection and stent implantation, 1 underwent nasojejunal feeding tube implement under endoscopy, 2 underwent cholangiography and drainage tube placement and 1 underwent percutaneous transhepatic cholangial drainage (PTCD). 7 patients merely received chemotherapy. 14 patients received surgical procedures combined with systemic chemotherapy.
There was significantly lower 3 year survival rate for no less than 3 months from AP onset to tumor diagnosis than < 3 months (p = 0.047; Fig. 6). The 1, 2, 3 and 4 year cumulative survival rates of patients with tumor-induced AP were 58.9%, 44.6%, 34.4% and 17.2%. The median overall survival was 495 days (interquartile range 190.12–799.88 days).
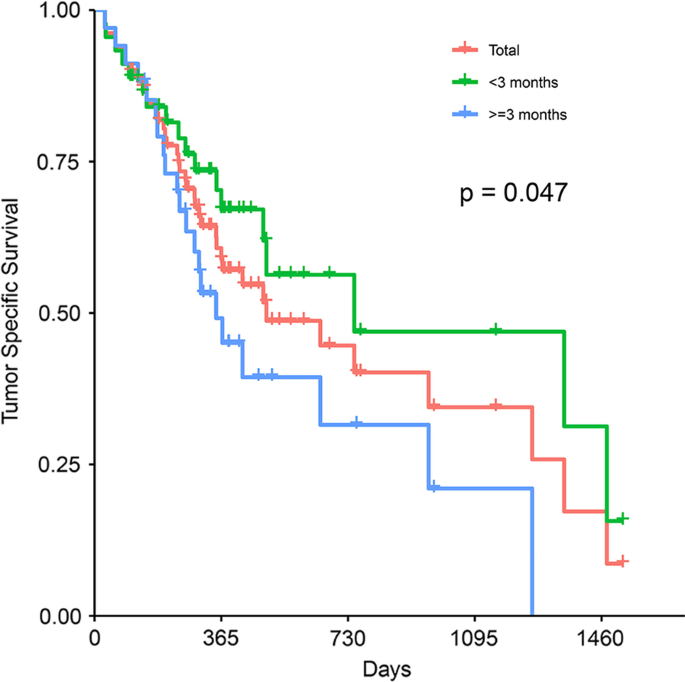
Kaplan–Meier curve for tumor specific survival of patients by whether the time from first attack of AP to tumor diagnosis was longer than 3 months or not



Comments
Post a Comment